Top 10 research highlights in 2021
Video produced by Melissa Parson
From vaccines to health equity, these are the research stories that made headlines over the last year
In 2021 …
- New vaccines began to protect us against COVID-19
- Health care organizations recommitted to health equity
- The work to improve management of chronic conditions and healthy aging continued
Kaiser Permanente Washington Health Research Institute contributed to these achievements and more in 2021. In this story and video, we highlight some of KPWHRI’s top research findings from the past year.
Expanding COVID-19 vaccine research
In March 2020, KPWHRI launched the first-ever clinical trial of a COVID-19 vaccine — what is now known as the Moderna vaccine. In 2021, we continued to be at the forefront of vaccine research. Our vaccine scientists, led by Lisa Jackson, MD, MPH, were part of a study that found the Moderna vaccine offered durable protection against Delta and other variants 6 months after vaccination. KPWHRI also joined a national clinical trial exploring mixing different vaccines and boosters.
In the meantime, KPWHRI scientists have also continued to work with the CDC (Centers for Disease Control and Prevention) and U.S. FDA (Food and Drug Administration) to monitor the safety of COVID-19 vaccines. A study published in October found that people who get a COVID-19 mRNA vaccine (Moderna or Pfizer-BioNTech) show no increased risk for a wide range of rare reactions that can sometimes occur after vaccinations. These findings were co-authored by Jennifer Nelson, PhD, KPWHRI’s director of biostatistics.
Pivoting to increase health care access
The COVID-19 pandemic has fundamentally changed how many of us access health care services. In the last year, KPWHRI scientists have continued to explore ways to provide timely, high-quality care in this challenging environment.
When the availability of mammogram appointments became limited due to the pandemic, KPWHRI researchers collaborated on a risk-based algorithm for prioritizing mammograms for individuals most likely to be diagnosed with cancer. Our researchers also worked with the Breast Cancer Surveillance Consortium to learn what concerned people most about returning for breast cancer screening, providing insights to help mammogram clinics adopt safety measures and expand access.
Providing care to low-income patients during the pandemic was the focus of a study looking at the use of telehealth services at safety-net health organizations in California. The researchers discovered that phone visits, not video visits, made up more than 90% of telehealth appointments during the first 6 months of the pandemic, reflecting patients’ personal, cultural, and privacy preferences as well as lack of access to digital communication technology. The study was co-authored by Maggie Jones, MPH, the director of the Center for Community Health and Evaluation (CCHE) at KPWHRI.
Advancing health equity
Our mission to improve health, well-being, and health equity for all communities took us in diverse directions in 2021.
Research conducted by CCHE demonstrated the value of health impact assessments to evaluate how proposed infrastructure projects, policies, and programs could affect the health and well-being of a community — timely findings given the recent passage of the $1 trillion federal infrastructure bill.
A KPWHRI-led study also took a close look at prediction models that use health record data to identify people at high risk of suicide, finding that models that work well in a general population sample can perform poorly in some racial and ethnic groups. Lead author Yates Coley, PhD, was recognized with the Paper of the Year award at the HCSRN (Health Care Systems Research Network) annual conference for this important research.
Improving breast cancer screening, diagnosis
Health equity was a central focus for our breast cancer researchers, too. A study led by KPWHRI collaborators found that race, income, and education may affect access to 3D mammography — technology that can improve breast cancer detection rates and decrease false alarms.
Other notable research found that having denser breasts continues to be a risk factor for women later in life, a finding that could help guide decision-making about breast cancer screening for women in their mid-70s and beyond. The study was co-authored by Weiwei Zhu, MS, and Diana Buist, PhD, MPH.
Contributing evidence about dementia prevention, intervention, and care
Healthy aging has long been a priority research area for KPWHRI, largely driven by Adult Changes in Thought (ACT) — a longitudinal study on aging and the brain that Kaiser Permanente Washington members have been contributing to for more than 30 years. ACT released major findings this year, including about associations between dementia risk and fine-particle air pollution, specific medications for high blood pressure, hearing loss, and cataract surgery.
Preventing suicide
This year, a Kaiser Permanente Firearm Injury Prevention Task Force study found that patients will answer a question about their firearm access during clinic visits. The study was led by Julie Richards, PhD, MPH, who also blogged about her personal motivation for studying this topic.
Other KPWHRI suicide-prevention research focuses on predicting risk of suicide attempt. For example, Rob Penfold, PhD, blogged about testing a machine learning algorithm for accurately predicting suicide risk in adolescents and youth.
Improving care for cardiovascular disease
A study conducted under real-world clinical conditions described barriers that small primary care clinics face in integrating risk calculators into cardiovascular care. The study was led by Leah Tuzzio, MPH, and a team who evaluated part of the Healthy Hearts Northwest project.
In hypertension care, the BP-CHECK study led by Bev Green, MD, MPH, found that study participants preferred home monitoring over other methods for tracking their blood pressure.
Changing our thinking about bariatric surgery, weight gain
New research found that bariatric (weight-loss) surgery may help people with chronic kidney disease (CKD) and obesity live longer — a finding that challenges earlier studies linking obesity to better survival among people with CKD (known as the “obesity paradox”).
Another study called conventional wisdom into question by suggesting that people don’t seem to gain or lose weight because they live near a fast-food restaurant or a supermarket. However, the researchers did find that living in a more densely populated, walkable neighborhood could have a small impact. The study was co-led by David Arterburn, MD, MPH, and University of Washington researchers.
Advancing chronic pain management
Cognitive behavioral therapy (CBT) that included adaptive yoga-based movement skills helped people on long-term opioid treatment manage chronic pain in a study led by Lynn DeBar, PhD, of Kaiser Permanente patients in Oregon, Georgia, and Hawaii. And a study with Kaiser Permanente Washington members found that phone-based CBT for insomnia helped older people with persistent pain from osteoarthritis sleep better.
Gaining from EHRs with insights on note-sharing, cannabis use
In April, a federal rule began requiring doctors to provide patients with virtual access to their online notes. For doctors concerned about this change, a KPWHRI study led by James Ralston, MD, MPH, provided reassurance, finding that doctors’ fears about allowing their patients to see notes in their electronic health record (EHR) diminished after first-hand experience with such access. Most providers also found that note-sharing was overall a benefit to patients despite continued concerns about worrying or confusing patients.
Sharing is a 2-way street, of course, and patients’ openness with their doctors about their cannabis use, as documented in their EHRs, allowed KPWHRI researcher Theresa Matson, MPH, and colleagues to estimate the extent of medical cannabis use and its overlap with health conditions, including conditions that may be helped or harmed by cannabis use.
We look forward to continuing our work to create a healthier, more equitable world in 2022, and we wish everyone a safe, healthy, and joyful new year.
New funding

Grant of over $55M to boost Alzheimer’s, dementia study
Kaiser Permanente Washington will co-lead an expanded ACT Program to better understand the aging brain.
ACT Center

New center focuses on equitable, whole-person health care
Kaiser Permanente launches the Center for Accelerating Care Transformation.
Co-designing with patients

Patient collaboration sparks care innovations
By partnering with patients, KPWHRI researchers developed 2 new interventions to boost lung cancer screening.
Drugs, diabetes, disparities
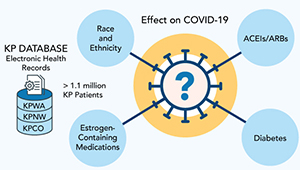
Studying COVID-19 risk and outcomes
Dr. Sascha Dublin tells how studies of KP electronic health record data can improve COVID-19 treatment and prevention.
2020 highlights

10 ways we helped chart a safer passage in 2020
KPWHRI responded to the COVID-19 hurricane with actions to improve health worldwide.
Top ten splashes from KPWHRI in 2019

Explore 10 ways that Kaiser Permanente Washington research has advanced health and health care this year
10 ways we made a healthier world in 2018

Kaiser Permanente Washington research tackled problems like obesity, suicide—and care that doesn’t promote health.



