New NIA grant of over $55M to boost ambitious Alzheimer’s, dementia study

J. Denis Watts, a participant in the Adult Changes in Thought study, has his balance tested during a visit with Becky Lederman, a research specialist at the research clinic at Kaiser Permanente Washington Health Research Institute.
Kaiser Permanente Washington, University of Washington, and University of California-San Diego will lead an expanded ACT Program to better understand the aging brain
The National Institute on Aging, part of the National Institutes of Health (NIH), has awarded a grant expected to total $55.6 million to diversify and broaden the participants and science of the Seattle-based Adult Changes in Thought (ACT) Study.
Over the last 3 decades ACT has enrolled and followed several thousand older adults who receive care as Kaiser Permanente Washington (KPWA) members. To date, the project has identified numerous factors that affect brain aging, with the aim of developing better ways to treat and prevent Alzheimer’s disease and dementia, while creating unique comprehensive longitudinal data sets from aging persons and their brains in a community setting.
Under the new 5-year grant, ACT personnel will expand the existing cohort of 2,000 KPWA members to 3,000. The enrollment effort will include new strategies to recruit a more diverse population. The study personnel will grow to 41 faculty members at 10 research institutions. Researchers will deploy the latest tools to analyze brain structure changes, to measure neuronal responses to a variety of drugs, and to evaluate cognitive and physical functioning. Also, as part of the grant, the ACT team will make its data more accessible to researchers nationwide.
“We have become a dynamic ‘living laboratory’ of aging,” said Eric B. Larson, MD, MPH, one of 3 ACT multiple principal investigators (MPIs) and a senior investigator at Kaiser Permanente Washington Health Research Institute (KPWHRI), where ACT was launched in 1994. “Thanks to the generosity of the ACT volunteers, we can investigate years of detailed medical records for study participants — often dating back decades before the study began because of their membership in Group Health [KPWA’s precursor] — and do state-of-the-art studies of the brains from those who consent to autopsy.”
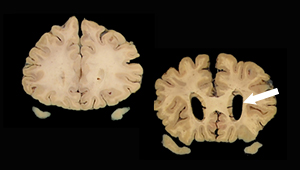
The study has established one of the world’s largest brain banks set in a community health care system dedicated to the study of the aging brain, Alzheimer’s disease, and dementia with more than 880 brains donated from ACT volunteers.
In addition to Dr. Larson, the 2 other ACT MPIs are Paul Crane, MD, MPH, professor of medicine at the University of Washington (UW) and Andrea LaCroix, PhD, professor and chair of epidemiology at the University of California, San Diego (UCSD).
Since ACT’s first cohort was established in 1994-96, new volunteers have been added as others die. Total enrollment is now more than 5,800 persons over 65 years old.
In dozens of studies, ACT researchers have identified and quantified numerous factors that affect brain aging, including early life exposures, education, hearing and vision loss, traumatic brain injuries, hypertension, alcohol consumption, obesity, smoking, depression and social isolation, physical inactivity, and blood sugar levels and diabetes. A few examples:
- Frequent exercisers had 38% lower incidence of Alzheimer’s disease and dementia as compared with those exercising 3 or fewer times per week.
- Higher glucose levels are associated with an 18% increased risk of Alzheimer’s disease and dementia in people without diabetes and a 40% increased risk in people with diabetes
- 47% of cognitively normal brains had substantial neuritic plaque density and 33% had microinfarcts, which runs counter to a widespread view that such markers are reliable indicators of Alzheimer’s disease and dementia.
- The study has linked a number of medications to higher risk for developing dementia.
The new ACT award — more than 3 times the amount of the current funding level — will support 3 distinct research projects. One examines relationships of 24-hour patterns of device-measured physical activity and sleep with brain aging and dementia. A second characterizes particular subtypes of Alzheimer’s disease to see whether they have different brain imaging or neuropathology findings, and whether people with these different subtypes have different experiences with dementia. A third will study the effects of particular commonly used drugs, which the ACT study has shown can influence dementia risk, on neuron cells grown from participant cells using state-of-the-art stem cell approaches.
The new program has a set of 6 cores — administrative, clinical, life course, neuropathology, neuroimaging, and data and analysis — that support the study and sharing of research data.
With the next round of funding, ACT has added a third MPI, Dr. LaCroix, professor and chief of epidemiology at UCSD, who was involved at the start of the study as a researcher in Seattle at Group Health’s Center for Health Studies, the precursor for KPWHRI. “As both an epidemiologist and the daughter of a mom now suffering from Alzheimer’s disease, I have a deep commitment to finding ways to improve brain aging,” said Dr. LaCroix, who is also a KPWHRI affiliate researcher. “We are all indebted to the ACT community participants past, current and future, who will be working with us on these discoveries over the next 5 years and beyond.”
The ACT team includes faculty and staff from KPWHRI, UCSD, Boston University, Columbia University, Swedish Medical Center in Seattle, University of California-Riverside, University of Pennsylvania, University of Toronto, University of Wisconsin-Madison, and 9 departments at UW.
Dr. Crane, who started working on ACT as a fellow at the UW Department of Medicine, where he is now a professor of medicine, said: “It is a privilege to work with this terrific team on important questions around aging and dementia. This next chapter of the ACT study builds on the tremendous generosity of our participants and the hard work of so many to pull together this proposal.” He is also a KPWHRI affiliate researcher.
ACT is funded by NIH grant number U19AG066567.
Kaiser Permanente issued a news release about this grant on Aug. 26, 2021.
Research
Study evaluates biomarker criteria for Alzheimer’s risk
One-third of people classified as ‘highest risk’ may not develop Alzheimer’s disease, study suggests
News
Seattle team to build brain map of Alzheimer’s disease
$40.5M NIH-funded project aims to pinpoint cells at root of brain disease—and new therapeutic targets.
healthy findings blog

New Lancet report offers hope for preventing dementia
Dr. Eric B. Larson, a report contributor, answers questions about reducing risks, disparities, and threats from COVID-19.
medication use
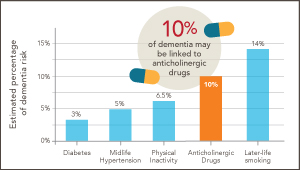
Could ‘deprescribing’ anticholinergic drugs prevent dementia?
Dr. Larson reflects on splashes, ripples—and new research by U.K. scientists, which builds on his earlier findings from the ACT study.


