Can machine learning help treat depression more effectively?

A new grant funds modeling work to make personalized treatment possible
The most commonly used depression medications have similar rates of effectiveness overall, but the response for individual patients varies widely. A medication that works well for one person might not work at all for another person, and clinicians don’t have good tools for predicting success ahead of time. This means that many patients try multiple options before finding something that improves their symptoms, a process that can take months.
With a new grant, researchers at Kaiser Permanente Washington Health Research Institute (KPWHRI) and their colleagues are hoping to find a better way. Their project will use machine learning methods to find patterns in how patients respond to antidepressants, with the goal of building a model that could make treatment more personalized — using information from a person’s health record to figure out which medication might be best for them.
“Most previous research has used short-term information from relatively small samples of people taking antidepressant medications,” said Gregory Simon, MD, MPH, senior investigator at KPWHRI and the lead researcher on the grant. “We hope that long-term data from much larger samples will allow us to identify patterns that previous research has not detected.”
The grant from the National Institute of Mental Health, for $800,000 over 3 years, will allow the research team to look at a large amount of data and leverage tools and methods from the Mental Health Research Network, a consortium of research centers across the country.
“Our study differs from previous work in some fundamental ways,” Simon said. “We’re looking at a large and diverse sample of people treated in real-world practice. We’re able to see multiple encounters with the health system and track people’s history with different medications.”
The study will include data from more than 250,000 patients receiving care in 4 large health systems: HealthPartners in Minnesota, and the Washington, Northern California, and Southern California regions of Kaiser Permanente.
The researchers will engage with patients, clinicians, and other health system partners to tailor their approach so that they can answer the most relevant questions with their study.
Part of the difficulty of personalizing depression treatment is teasing apart factors that impact someone’s response to a specific medication from those that might influence their outcome with any medication — or have an impact on whether they receive treatment at all. For example, researchers know that things like co-occurring conditions and demographic characteristics affect someone’s likelihood of seeing an improvement in their depression symptoms. However, the relationship between those factors and someone’s response to an individual medication is unknown.
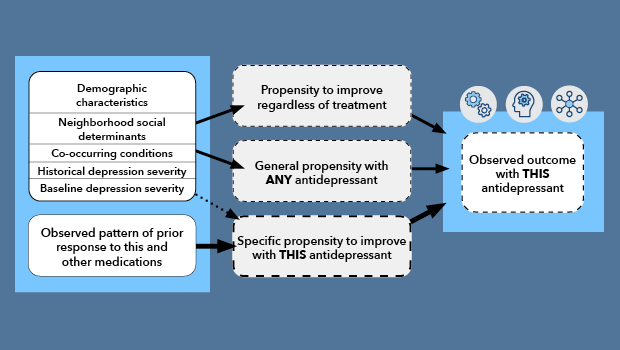
A diagram shows a conceptual model for detecting specific treatment effects. Propensity to respond favorably to a specific medication is currently unobservable, but may be indicated by observed patterns of prior medication response (bold arrows). Historical, environmental, and baseline clinical characteristics are known to influence overall prognosis and response to any medication (solid arrows) and may influence a response to a specific medication (dashed arrow).
“We’re tackling several different things with this study,” Simon explained. “We’re going to test previous assumptions about personalized treatment, and we’re going to seek to identify new rules for personalization that can be used in clinic.”
By drawing on long-term data of how people have responded to medications in the past — as well as patient characteristics like socioeconomic status, insurance coverage, and unmet social needs — the study team hopes to bring more clarity to depression treatment and help clinicians and patients find a successful course of treatment more quickly.
“Every year, more than 10% of people in the U.S. are taking medication for depression,” Simon said, “and around half of those people won’t see improvement with the first medication they try. So, this has the potential to impact a lot of people’s lives.”
HealthPartners, Kaiser Permanente Northern California, and Kaiser Permanente Southern California are research partners on the grant.
By Amelia Apfel
Research

Improving and advancing mental health care
KPWHRI researchers are contributing to better mental health care for people nationwide.
New findings

Simpler models to identify suicide risk perform similarly to more complex ones
Models that are easier to explain, use could have better uptake in health care settings.
Research

A medication that can relieve symptoms of psychosis is underused
Study finds that many patients who might benefit from clozapine don’t receive it.



