Using texting, stories to increase screening for colorectal cancer
Video produced by Melissa Parson
Addressing barriers can help more people complete screenings on time
Colorectal cancer is the second most deadly type of cancer in the United States, according to the National Cancer Institute. Only lung and bronchus cancer kills more people each year. However, colorectal cancer is also highly preventable with regular screening, and if the cancer is caught early and hasn’t spread, survival rates are high.
Evaluators at the Center for Community Health and Evaluation (CCHE), part of Kaiser Permanente Washington Health Research Institute, found that a quality improvement project encouraging people overdue for colorectal cancer screening to mail back a home screening kit helped increase screening rates. The project used bidirectional texting, where recipients can respond and engage in a conversation, and sent stories in the format of fotonovela comics to engage patients and provide education about the importance of screenings. Nearly 40% of patients who received the texts engaged with them, and those who engaged had higher screening rates than those who did not. The results were published this month in JMIR Cancer. The evaluators also interviewed a subset of patients, who shared feedback on challenges and barriers to screening, providing insights to help improve the program.
“The strategies used in this intervention build on prior work from our clinical partners to understand barriers that prevent patients from changing their behavior,” said Carly Levitz, MPH, lead author of the paper and an evaluation and learning associate at CCHE. “The results of our evaluation are helping our clinical partners refine and adjust the intervention to make sure that they are reaching as many patients as possible with messages that resonate and motivate them to get screened for cancer.”
Testing the intervention
The intervention was tested at AltaMed, a Federally Qualified Health Center in California, which serves a population that is majority Hispanic or Latin American. Compared to non-Hispanic white patients, this population is less likely to be screened for colorectal cancer and more likely to be diagnosed with advanced disease.
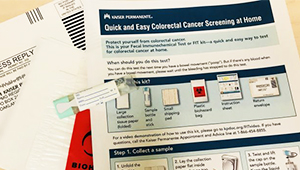
As part of routine care, the health center mails fecal immunochemical tests, or FIT kits, to patients who are due for screening. The health center also texts patients who receive a mailed kit to provide instructions and a follow-up reminder. FIT kits use a stool sample, which can be collected at home, to screen for colon cancer. For asymptomatic adults at average risk, the U.S. Preventive Services Task Force considers them to be as effective as a colonoscopy when done annually.
For the quality improvement project, evaluators randomized 5,241 patients who had not completed their FIT kit after 12 weeks into 2 groups. One group received the intervention, which consisted of an additional 4-week series of text messages that were automated and monitored using a program developed by mPulse Mobile. Through a natural language understanding platform, patients received replies when they responded to the texts. The participants could opt out at any point and would not receive any further messages. They received texts in their preferred language, either English or Spanish. In combination with the text messages, participants were sent a link to a fotonovela in either English or Spanish, containing a comic about someone encouraging a friend to complete their FIT kit and explaining why the screening is important. The second group (the control group) did not receive additional outreach.
“The texts and automated responses are designed to address known barriers and motivate people to complete the FIT kit,” said Elena Kuo, PhD, MPH, a co-author of the paper and a senior evaluation and learning consultant with CCHE. “In the first week, we focused on reminding people of the reasons to get screening done. The second week, the text asked patients to tell us if there were specific reasons why they hadn’t yet been screened — things like being too busy, being scared of the results, or not being sure why they needed to do it. We sent tailored motivational responses using natural language understanding that addressed their responses. We also sent fotonovelas and provided a final reminder in the last week about getting the FIT kit back to the health center.”
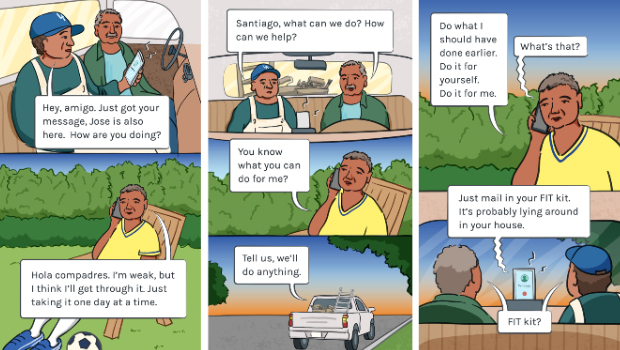
Panels from a fotonovela comic sent to patients to encourage them to complete their FIT kit, a home screening kit for colorectal cancer
What did the evaluation find?
In total, 40% of patients who were part of the intervention group engaged with the text messages. Of those, 31% clicked on the link to view the fotonovela. The intervention group had a screening rate of 18.8%, while the group that did not receive the texts and fotonovela had a screening rate of 11.7%. Screening rates were higher among patients who engaged with the text messages than among those who did not.
Evaluators found that older patients (ages 61 to 75) were less likely to engage with the text messages than patients ages 50 to 60. Language preference, insurance type, and a social determinants of health index score (a measure of whether someone lives in a low-needs or high-needs area) also were associated with text engagement. At the end of the intervention, women, Spanish speakers, and those with an inconsistent screening history (compared to very inconsistent or never screened) were more likely to have completed their FIT kit.
CCHE staff also conducted interviews with a sample of 16 patients from the intervention and control groups, who both did and did not return a FIT. People who participated in the intervention reported feeling that it was not invasive, and they were not bothered by receiving the text messages in addition to the usual reminders sent by the health center.
Participants reported several barriers to completing their FIT kit. The most common barrier identified in text responses was patients answering that they felt fine and didn’t have symptoms. Other responses were that patients weren’t sure why they needed the screening or that they were too busy. A few patients answered that it was embarrassing to complete the kit. For interviewees, the most common barrier was forgetting to complete their FIT kit. Other answers included not wanting to take the time to do it, losing the kit, or not remembering having ever received it.
“Addressing barriers is critical to improving screening rates, particularly for our most marginalized populations,” Kuo said. "Screening remains one of the most important preventive tools for improving health outcomes. While this campaign did increase screening rates, there’s still so much room for improvement, and so we appreciated the feedback from participants about what’s working and what remains a challenge.”
The patients interviewed said that mailing the FIT kits to their home was preferable to visiting the clinic for screening. They found the instructions helpful but suggested offering more support to people completing the FIT kit for the first time. Some interviewees proposed adding a small incentive as a way to get more people to complete the kits.
“Our results emphasize how important it is to make sure that educational materials and health promotion campaigns are designed with patients in mind, and co-designed with patients whenever possible,” Levitz said. “For example, we observed that patients aged 61 to 75 years were less likely to engage in the text messaging than patients who were aged 50 to 60. So, that tells us that there might be other strategies needed to reach the older age groups, and we need to be careful that health promotion campaigns don’t leave them out.”
The evaluators highlighted several directions for future work. They suggested looking further at the most impactful timing for targeted texting campaigns (relative to when patients receive their FIT kit), as well as studying unidirectional texting (recipients can’t respond to texts), which is less resource-intensive for a health care organization to implement. The results showed that the fotonovelas were not responsible for increasing screenings above and beyond the bidirectional texting, but they might have a different impact if included with unidirectional texting. AltaMed has been looking at options ahead of this year’s screening campaign, hoping to reduce barriers and continue to maximize impact and health outcomes for patients.
By Amelia Apfel
CCHE

Learn more about Center for Community Health and Evaluation
CCHE helps you find out what works to make communities healthier.
healthy communities

30 years of evaluations to improve community health
CCHE is devising new ways to find the interventions that most benefit community health and how best to measure them.
Healthy findings blog

Preventing heart attacks, strokes through health management
How the PHASE program improved care for people at risk of cardiovascular disease.
Research to practice
Making colon cancer screening easier for patients
KPWHRI’s Kilian Kimbel reflects on how the SOS study helped pave the way for a new program to find colon cancer early.


