$10 million grant to expand Mental Health Research Network
The NIMH awarded a third round of funding, enabling the MHRN to conduct larger studies in integrated health systems on topics that matter most.
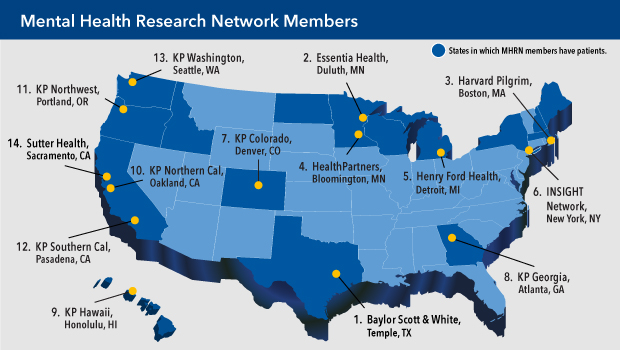
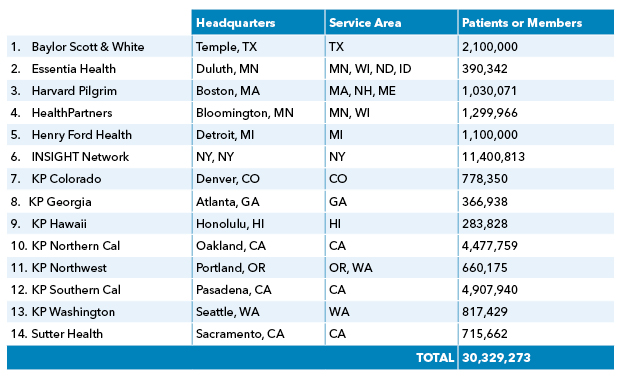
The National Institute of Mental Health awarded in November a 5-year $10 million grant to the Mental Health Research Network (MHRN), a consortium of 14 research centers affiliated with the nation’s largest integrated health systems. Launched in 2010 under the direction of Greg Simon, MD, MPH, Kaiser Permanente Washington Health Research Institute senior investigator and a Kaiser Permanente Washington psychiatrist, the MHRN has pioneered new ways to use electronic health records to improve how providers identify patients with mental health disorders and promptly deliver the most appropriate treatments.
With the new grant, the network will add new partners, increasing the diversity and size of the populations it studies ─ now totaling more than 30 million patients ─ as well as having more resources to devise trials using advanced machine learning and other new analytic methods. We asked 7 questions to Dr. Simon, the MHRN principal investigator, to get an overview of what the consortium has accomplished to date and what research he foresees it conducting in the coming years.
Q: What do you see as MHRN’s major achievements in its first decade? Can you offer some specific examples of ways that it has improved care?
Greg Simon: Our work to identify and address risk of suicide or self-harm has truly transformed research and health care delivery. I can honestly say we have moved the boundary of what seems possible in terms of identifying people at high risk for suicidal behavior and implementing effective suicide prevention strategies across large health systems.
Q: How does the new grant enable the MHRN to grow?
GS: The INSIGHT network, led by Dr. Rainu Kaushl of Weill Cornell Medicine, is joining MHRN. INSIGHT includes several large health systems serving over 11 million patients in the New York City area. This addition will nearly double the size and increase the diversity of the MHRN member/patient population. The INSIGHT network includes a diverse range of health systems, including safety-net providers serving large numbers of uninsured people. That fills in an important gap in our network.
Q: Why is it important to have MHRN continue? What does it bring to the table that is unusual, if not unique?
GS: We aim to be a national resource to improve mental health care. Our community brings together patients, researchers, health plan leaders, medical group leaders, and government officials to identify and rapidly address high-priority questions. We are fully embedded in real-world health systems. That allows us to ask the right questions and rapidly implement the answers.
Q: Is there a new role for patients in this research?
GS: Patients or mental health services consumers will serve as full members of the MHRN Steering Committee. MHRN has always emphasized engagement with patients in setting research priorities, but this change more clearly recognizes patients’ role in leading our network. This formalizes a principle that we’ve believed in but hadn’t previously formalized. We have always valued what patients had to say about research; now we are providing them with the same voting power as the researchers.
Q: What new research projects does the grant make possible?
GS: MHRN includes over 20 active research projects, and several include collaborations with health systems outside our network. This new funding will support four specific projects: a large pragmatic trial of mindfulness-based therapy for depression in pregnancy, an evaluation of patient and clinician views about use of algorithms or prediction models in suicide prevention, an evaluation of how new medications for depression affect risk of suicide attempt, and testing of an outreach program to reduce racial and ethnic disparities in starting treatment for depression.
Q: What does the award allow you to do in terms of improving analytical methods?
GS: Work on machine learning or artificial intelligence is too often focused on the newest tools rather than the practical jobs that need to be done. We aim to apply the most advanced analytic methods, such as machine learning, to questions that actually matter in clinical care. We aim to match the most effective tools with the most important jobs. We are not committed to any specific tools. Instead we focus on what patients, clinicians, and health systems need.
Q: Anything else you’d like to add?
GS: I hope that our overall research program looks very different five years from now. That will mean that we are identifying and addressing new questions, rather than just re-hashing old ones.
healthy findings blog
From 17 years to 17 months: Accelerating implementation
Dr. Greg Simon tells why adopting new suicide-prevention findings avoided delays that plague research implementation.
recognition

Dr. Greg Simon wins national suicide prevention award
Kaiser Permanente physician-scientist will receive American Foundation for Suicide Prevention's Lifesavers Research Award.
suicide prevention

Suicide prevention: Research network finds new way to predict risk
Led by KPWHRI scientists, study aims to target those who need interventions most.



