What's new in cannabis use research?
Use in pregnancy and screening in primary care studied by KPWHRI’s Kiel, Matson, and Lapham
Legal cannabis is expanding in the U.S. — 21 states and the District of Columbia allow sales to adults over age 21. Washington state and Colorado were the first to legalize nonmedical use, in 2012. Three years later, Kaiser Permanente Washington began adult behavioral health screening in primary care, based on research from Kaiser Permanente Washington Health Research Institute (KPWHRI). The screen contains a single question about frequency of cannabis use.
“In a state with legal cannabis use, it's important that primary care providers have knowledge of patient cannabis use. The single-item cannabis question has also been integral to advancing our understanding of how and why patients use cannabis,” said Gwen Lapham, PhD, MPH, MSW, KPWHRI assistant investigator, who leads research in this area. Three recent studies are summarized below.
Use in pregnancy
KPWHRI Project Manager Linda Kiel authored a paper based on interviews of pregnant women who reported cannabis use on the primary care screen. The study goal was to gain insights into cannabis use and decision-making during pregnancy. The results, in Preventive Medicine Reports, showed that all 15 interviewees wanted information about cannabis use during pregnancy. They asked friends and family and searched the internet but found little conclusive evidence about risks or benefits. Interviewees expressed reluctance to discuss the topic with their medical provider because of fear of judgment.
Interviewees often used cannabis medically, such as to treat morning sickness, or alleviate mental health symptoms or pain. Common reasons for not using cannabis were uncertain risks and a partner who was against it. Participants were mainly comfortable with their cannabis use, but some worried about potential long-term consequences of cannabis use for their child. Those who breastfed reported concerns and uncertainty about how cannabis might affect their baby.
The researchers concluded that health care organizations must be proactive about screening and counseling in this area. “Cannabis use during pregnancy isn’t uncommon,” Kiel said, “and some research suggests fetal risks, so medical providers should be aware about reluctance to discuss cannabis use in a clinical setting. They should understand the varied reasons for cannabis use during pregnancy, be ready for conversations about the risks, and support evidence-based choices."
Kiel’s coauthors, all from KPWHRI, are Clarissa Hsu, Paige Wartko, Ladia Albertson-Junkans, John Ewing, and Gwen Lapham.
Use for medical reasons
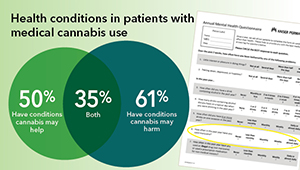
Lapham led a study that confidentially asked nearly 1,700 adult Kaiser Permanente Washington primary care patients about cannabis use, with a survey that provided in-depth data. Results are in JAMA Network Open, showing that 39% of survey respondents reported past-year cannabis use.
The survey asked explicitly if cannabis use was for medical reasons and it also asked indirectly, with a question about whether the patient had health reasons for use. Among primary care patients, 27% reported explicit medical use, and 35% reported health-reason use, primarily for pain, sleep, stress, anxiety, and depression.
The study team compared the results to information in the electronic health record (EHR) and found that it missed most medical cannabis use: the EHR, including clinician notes, showed only 5% of patients with any documentation of medical or health reasons for cannabis use. “Most of the primary care patients we surveyed used cannabis for medical reasons,” said Lapham. "But only 10% of survey respondents who reported this use had it in their EHR.“
Alongside routine cannabis screening, asking patients about use of cannabis to manage health would improve recognition of medical use and the management of health conditions for which cannabis is being used, Lapham said.
Lapham’s KPWHRI coauthors are Tessa Matson, David Carrell, Jennifer Bobb, Casey Luce, Clarissa Hsu, Malia Oliver, and Katharine Bradley. Other coauthors are Udi Ghitza, Kendall Browne, Ingrid Binswanger, Cynthia Campbell, Andrew Saxon, Ryan Vandrey, Gillian Schauer, Rosalie Liccardo Pacula, Michael Horberg, Steffani Bailey, and Erin McClure.
Risk of cannabis use disorder
Of 50 million people in the U.S. who use cannabis, some have or are at risk for cannabis use disorder (CUD). This is an inability to stop using cannabis, even when it causes harm such as anxiety or mood or memory problems. Because frequent cannabis use can increase risk of CUD, primary care screening could help health care teams recognize patients who need additional CUD assessment.
Collaborative Scientist Tessa Matson, PhD, led a study validating the single-item screen about cannabis use frequency, asking: When administered routinely in primary care and documented in the EHR, could it identify people with potential CUD risk? Possible CUD was determined using the same survey as the Lapham study, which included 15 validated items considered the gold standard for measuring CUD. The researchers tested how well different frequencies of cannabis use, assessed by the single-item screen, predicted the probability of CUD.
Results are in JAMA Network Open: Nearly 7% of the survey sample met criteria for possible past-year CUD. The single-item screen for cannabis use performed excellently, with predictive values that reflected the cannabis use frequency and general level of CUD in the screened population.
Health organizations interested in screening for possible CUD can tailor the screening thresholds for their population and level of follow-up care they can provide. A health organization serving people with higher risks of substance use disorders might provide additional assessment for patients reporting any cannabis use, while another whose patients have lower general risk might additionally assess only those reporting daily use.
“A single question is effective at helping health care organizations find out who might be helped by additional CUD screening,” Matson said. “It can easily be added to other questions asked during primary care visits.”
Matson’s KPWHRI coauthors are Gwen Lapham, Jennifer Bobb, Malia Oliver, Emily Williams, and Katharine Bradley. An additional coauthor is Kevin Hallgren.
By Chris Tachibana
New findings

Research roundup on natural language processing and machine learning
Using doctor's notes to learn about drug reactions, dementia, and cannabis use.
Electronic health records
EHR study offers insights on medical cannabis use
New research examines providers’ notes to understand patients’ cannabis use and health conditions.
Innovations in care

Alcohol and drug use care goes virtual with COVID-19
Kaiser Permanente Washington researcher Joe Glass advises integrating digital prescriptions into existing care.


