Is bariatric surgery helpful in chronic kidney disease?
In an Annals of Surgery study, Kaiser Permanente researchers and colleagues share findings that bariatric surgery is linked to lower death risk in persons with chronic kidney disease and obesity
By David Arterburn, MD, MPH, senior investigator at Kaiser Permanente Washington Health Research Institute and internal medicine physician at Kaiser Permanente Washington
There aren’t many things that can prolong life in patients with chronic kidney disease (CKD) — but it appears that bariatric surgery is likely to be one of them for people with both CKD and obesity.
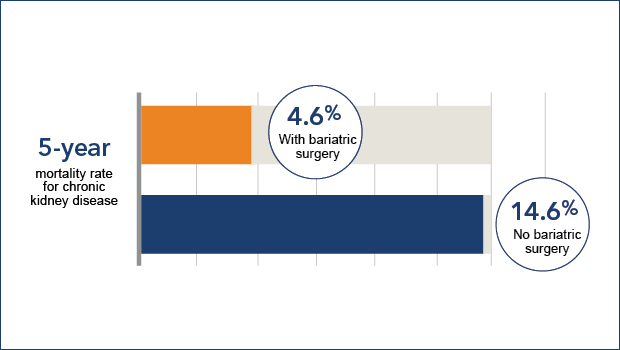
In our recent study, led by Karen J. Coleman, PhD, and published in Annals of Surgery, we found bariatric surgery was associated with a 79% lower 5-year risk of mortality, when a sample of adults with CKD and obesity who had a weight-loss operation were compared with a similar group of adults who did not undergo such a procedure.
This is the latest in a series of papers by our research team documenting how bariatric surgery’s benefits appear to extend beyond weight loss — showing in many instances that the risks of harm from the surgery are often substantially less than the risks of not having it.
We have found, for instance, that diabetes goes into remission for an average of 7 years in people who have gastric bypass surgery, a common type of bariatric surgery. Our research has also found that bariatric surgery is associated with fewer heart attacks and strokes — and less eye, kidney, and nerve disease — in people with diabetes and severe obesity.
CKD, a condition characterized by a gradual loss of kidney function over time, affects 15% of adults worldwide and is associated with reduced life expectancy. Compared with the general population, the independent risk of death is 490% higher in individuals with advanced CKD. Unfortunately, few therapies have been shown to reduce mortality in these individuals, and more research is needed to improve treatment.
In multiple prior observational studies of patients with CKD, obesity has been associated with better survival; a phenomenon known as the obesity paradox. Controversy over whether obesity increases or lowers risk of death is a major impediment to optimizing CKD management.
My colleagues and I conducted a retrospective cohort study examining risk of all-cause mortality among 802 patients with CKD and severe obesity who had bariatric surgery compared with 4,933 matched patients who didn’t have the surgery.
The 5-year mortality rate in control patients with CKD and severe obesity was very high: 14.6%, or 1 in 7 died within 5 years. In contrast, among those that had bariatric surgery, the 5-year mortality rate was 4.9%, or only 1 in 20 died within 5 years.
Although there is modest increased perioperative risk in patients with CKD undergoing bariatric surgery, we found a large long-term protective effect of surgery on mortality that appears to far outweigh this short-term risk.
The prevalence of obesity has been steadily growing in the past several decades, but there is reason to be optimistic that we can reverse that trend. Along with advances in understanding how body weight is regulated and how human psychology drives our behaviors, we are learning more about the appropriate use of bariatric surgery. Currently only 1% to 2% of all eligible patients undergo such surgery each year; my colleagues and I believe bariatric surgery can play a greater role for select patients with obesity who stand to benefit the most from those treatments. However, behavioral treatments will likely remain the primary approach to obesity, and there is growing evidence that pharmacological treatments will play a greater role in obesity treatment as well.
Our most recent results challenge the obesity-CKD paradox paradigm and support the use of bariatric surgery to improve the survival of patients with CKD and severe obesity. Patients with CKD and severe obesity should be having conversations with their doctor about whether or not bariatric surgery is a reasonable treatment option for them.
The study, “Bariatric surgery and risk of death in persons with chronic kidney disease,” was published March 3, 2021 in Annals of Surgery. Its lead author is Karen J. Coleman PhD, of Kaiser Permanente Southern California, Department of Research and Evaluation. The co-authors are Yu-Hsiang Shu, PhD, Heidi Fischer, PhD, Tae K. Yoon, MPH, Brianna Taylor, MPH, Talha Imam, MD, and Stephen DeRose, MD, of Kaiser Permanente Southern California; Eric Johnson, MS, Mary Kay Theis, MS, and David Arterburn, MD, MPH, of Kaiser Permanente Washington Health Research Institute; Lisa J. Herrinton, PhD, David Fisher, MD, Robert A Li, MD, and Liyan Liu MS, of Kaiser Permanente Northern California; David H. Smith, PhD, of Kaiser Permanente Northwest; Sebastien Haneuse, PhD, of Harvard T. H. Chan School of Public Health; Anita P Courcoulas, MD, of University of Pittsburgh Medical Center; and Allon N. Friedman, MD, of Indiana University School of Medicine. This research was funded by a National Institute of Diabetes and Digestive and Kidney Disorders (NIDDK) award #R01DK105960 granted to Drs. Arterburn and Coleman.
research

Weight loss lasts long after bariatric surgery
Diverse Kaiser Permanente patients maintained weight better after gastric bypass than after sleeve gastrectomy
research

Can you lose and maintain weight by eating mindfully?
Robin Garcia and David Arterburn’s personal and professional paths converge in a pilot project.
Healthy Findings Blog

We decreased people’s daily sedentary time by an hour
Changing behavior isn’t easy, but Dr. Dori Rosenberg helped older people to stand and walk more.
medication safety

Using phentermine for weight loss longer term found to be safe, effective
Dr. David Arterburn discusses reassuring news from his PCORnet study of the most widely used anti-obesity drug in the United States.


