Watch our new video, ‘Research for the rest of us’
Drs. Neely Williams and David Arterburn talk about how important patient involvement is to the PCORnet Bariatric Study
Neely Williams, MDiv, EdD, PCORnet patient co-principal investigator and community principal investigator for the Meharry-Vanderbilt Alliance, and David Arterburn, MD, MPH, a senior investigator at Kaiser Permanente Washington Health Research Institute and an internal medicine physician at Kaiser Permanente Washington, discuss the importance of patient involvement in the PCORnet Bariatric Study, funded by the Patient-Centered Outcomes Research Institute. The video and transcript are by Melissa Parson, MFA, video producer at KPWHRI.
Someone with diabetes can tell you what it feels like
Dr. Williams: I'm always a proponent for listening to those that have had the experience and answering questions that are important to them. No one can tell you more about diabetes than the person who lives with it. Scientists may have a better understanding of the chemical makeup of the things that cause it, but it takes someone with diabetes to tell you what it feels like when you wake up in the morning or when you put your feet on the floor and pain starts to shoot through your feet from neuropathy.
We have a beautiful opportunity here to raise the banner in the community, to be able to say, “Here am I, and here are others,” who are participating in the process, and are demanding that we no longer be left out of the process when it comes to the research that's being done about the issues we face every day.
Dr. Arterburn: We were able to have patients in the room as we're designing the study, as we're asking the research questions, as we're formulating the analyses. One of our co-principal investigators, Neely Williams, helped us to think through what are the most important questions for patients, and to think through how we best disseminate the evidence to patients in a way that will have the greatest impact.
Dr. Williams: There was a time in my history where I first started to investigate the possibilities of having bariatric surgery, and that's when I started to see what other options I had. I sought out all the information that I could. It was very scary to think about having this surgery that would restructure my digestive tract. And I think it was because I had information both from primary [care] doctors as well as from surgeons, which did not always match. Primary [care] doctors seemed to express more of what the dangers were, whereas the surgeons stressed more of what the benefits were.
I am very excited about what PCORI brings, the change it’s bringing to the landscape of research. It is making patients center to the clinical research process. It's research for the rest of us. Those of us who have felt like we were not part of the process early on. The underserved, underrepresented communities have the opportunity to create new truths in medicine. Research is not a one size fits all. In fact, most ladies will tell you that most of the things that have been designed that say “one size fits all” doesn't fit everybody. So, certainly that's not true for research either.
Patients influence the research
Dr. Arterburn: I think the best example of how patients influence the course of this study is that when we first got the funding announcement from the funder asking for us to address these research questions, the questions they were most interested in were, “What impact does bariatric surgery have on weight loss and diabetes outcomes.” When we brought that to our patient partners on the research team, what they said is, “Those are really important questions, but what we really want to hear as well is how safe are these procedures compared head to head?” And so that question was incorporated into our research study as a third aim within our project, and was elevated to be a separate analysis, which was driven entirely by patient feedback.
Dr. Williams: The stakeholders were involved in not only the analysis itself, but the translation of the analysis into language that can be used to increase the decision-making process between physicians and patients.
Dr. Arterburn: As we're interpreting the results, we make sure we put it in language that patients can understand. And they're right here on our team to inform us what makes sense to them, and what doesn't.
Communicating across different cultural understandings
Dr. Williams: I worked diligently with the lay summary, to make sure that the language was palatable both for community and for researchers. We did not need cartoons, but we definitely needed a language that was communicating across different cultural understandings. It is difficult, in my particular community, where there are many people facing so many obstacles and challenges every day. You know, sitting down and having a conversation with them about research that may be impacting their lives every day, belonged far down the list.
When people are concerned about how they're going to get their medicines, how they're going to pay their bills based on the income they have, what's going to be cut next from their programs that will not allow them to be able to thrive in their living situation—and when you come to them, to the table and start talking about, “This is an opportunity for you to be engaged in research,” it may not come across as something that's important to them. So, what I would love for the community to understand is how research really does matter.
This can be done
Dr. Williams: I would like to continue to communicate to researchers, “This is something that can be done.” I do not assume that all researchers do not value the process or the activity of having someone involved. But I think there's a lot of hesitancy around how this impacts my progress, how this slows down my study. I think, ultimately, if we understand, as researchers understand, and if communities and patients understand, that we're working for the same end: better outcome from the research that's being done, the dollars that are being spent to do the research, and the time and the energy and the effort. If we could understand that we are all on the same page, and know that we're all looking for the same end goal, then it would help researchers to be more open to the process.
And I think it behooves those of us who are participating in lifting this banner to educate, educate, educate; not just patients and community people, but also researchers. And they can find that community is truly an asset, or a patient is truly an asset, because they definitely bring with them their wisdom and their expertise of the disease they're facing.
video

Which type of surgery has best weight-loss results?
Largest long-term study from PCORnet has answers for people with severe obesity. (Vimeo, 1:56)
obesity research
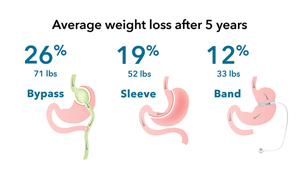
Gastric bypass surgery is best for weight loss for severe obesity
Largest long-term national study of bariatric surgery, comparing 3 most common operations, is among first PCORnet® results
Obesity & adolescents

Kaiser Permanente Researchers Study Bariatric Surgery for Obese Teens
In this Q&A, Dr. David Arterburn describes findings from the largest study in adolescents to date.


